The Immune Cost of Chronic Gum Inflammation2h ago
2h ago
Chronic gum inflammation is far more than a localized oral issue — it is a persistent immune challenge that places stress on the entire body. When gum tissue remains inflamed, the immune system must continuously respond to bacterial invasion, triggering systemic inflammation and weakening immune resilience over time. This article explores the biological mechanisms behind periodontal inflammation, its immune costs, and how precision oral care supported by AI-guided brushing can reduce inflammatory burden and protect long-term health.

Understanding Chronic Gum Inflammation
Gum inflammation — medically referred to as gingivitis or periodontitis — occurs when plaque bacteria accumulate along the gumline and trigger an immune response. While early inflammation may seem minor, chronic exposure leads to sustained immune activation.
Unlike temporary inflammation, chronic gum inflammation:
• Persists for months or years
• Continuously stimulates immune defense
• Damages surrounding tissues
• Creates systemic inflammatory signaling
The immune system is not designed for constant activation. Long-term stimulation comes at a biological cost.
How Gum Inflammation Burdens the Immune System
Continuous Immune Activation
Inflamed gums release inflammatory mediators that signal immune cells to remain active. This ongoing response diverts immune resources away from other protective functions.
Increased Systemic Inflammation
Oral bacteria and inflammatory molecules can enter circulation, elevating whole-body inflammation markers. This contributes to immune fatigue and reduced resilience.
Tissue Breakdown and Repair Demand
The immune system must constantly repair damaged gum tissue, consuming metabolic and cellular resources that would otherwise support healing elsewhere.
The Systemic Consequences
Research increasingly links periodontal inflammation with broader health outcomes, including:
• Cardiovascular complications
• Metabolic imbalance
• Elevated inflammatory load
• Reduced infection resistance
• Slower recovery from illness
While gum disease is not always the root cause, it is a measurable contributor to immune stress.
Why Gumline Cleaning Matters Most
The gumline is where plaque biofilm accumulates most aggressively. Unfortunately, it is also the area most frequently missed during brushing.
Incomplete cleaning leads to:
• Persistent bacterial colonies
• Micro-injury to gum tissue
• Recurrent inflammation cycles
This is why technique — not just frequency — determines immune impact.
How Smart Brushing Reduces Immune Load
AI-guided oral care technology helps eliminate inflammation triggers at their source.
BrushO Provides
• Pressure Monitoring
Prevents aggressive brushing that worsens inflammation
• 6-Zone × 16-Surface Coverage Tracking
Ensures full gumline cleaning
• Habit Reports
Identifies missed areas contributing to inflammation
• Adaptive Modes
Gentle settings for sensitive or inflamed gums
By improving plaque removal consistency, BrushO reduces microbial triggers that stimulate immune stress.
Preventing Chronic Gum Inflammation
Evidence-based strategies include:
• Thorough twice-daily brushing
• Daily interdental cleaning
• Balanced nutrition
• Hydration for saliva support
• Professional dental evaluations
• Smart feedback-guided brushing
Small daily improvements dramatically lower the inflammatory burden.
Chronic gum inflammation is not merely a dental inconvenience — it is an ongoing immune cost that affects whole-body health. Persistent oral inflammation keeps immune defenses engaged, reduces resilience, and contributes to systemic stress. Through precise plaque control and real-time guidance, smart oral care tools like BrushO help eliminate inflammation triggers before they become chronic. Protecting your gums ultimately protects your immune strength, longevity, and overall wellness.
最新の投稿
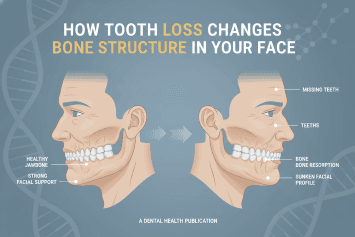
How Tooth Loss Changes Bone Structure in Your Face
Learn how tooth loss affects facial bone structure, jaw stability, and appearance. Discover prevention strategies and smart oral care tools to protect long-term oral health.
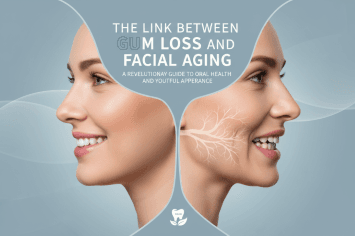
The Link Between Gum Loss and Facial Aging
Discover how gum recession contributes to facial aging, jaw structure changes, and smile aesthetics. Learn prevention strategies and smart oral care solutions.
How Antibiotics Permanently Change Your Mouth
Learn how antibiotics reshape your oral microbiome, affecting bacteria balance, gum health, and breath. Discover how to protect your mouth after antibiotic use.
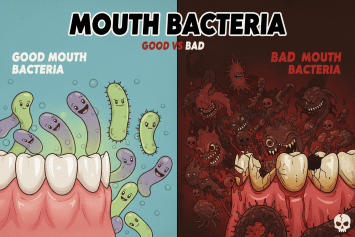
Good vs Bad Mouth Bacteria
Discover the difference between good and bad mouth bacteria and how maintaining oral microbiome balance protects teeth, gums, and overall health through proper hygiene and smart brushing.
The Immune Cost of Chronic Gum Inflammation
Chronic gum inflammation weakens immune defenses and increases systemic disease risk. Learn how periodontal inflammation impacts immunity and how to protect oral health.
Why Frequent Mouth Infections Signal Immune Weakness
Frequent mouth infections may be a warning sign of immune system weakness. Learn how oral infections reveal hidden health risks and how to protect your immunity.
Can Mouth Bacteria Affect Mood and Anxiety?
Emerging research shows that oral bacteria can influence mood, anxiety, and emotional balance through inflammation and the gut–brain axis. Discover how oral health impacts mental health.
How Oral Inflammation Affects Brain Fog and Memory
Oral inflammation doesn’t just damage your gums — it can disrupt brain function, trigger brain fog, and weaken memory. Discover how gum disease and oral bacteria affect cognitive health and how to protect your mind through smarter oral care.

Should You Brush Before or After Taking Vitamins?
Should you brush before or after taking vitamins? Learn how supplements affect enamel, saliva, and bacteria — and how smart brushing with BrushO protects your teeth.
The Unexpected Link Between Oral Health and Skin Breakouts
Discover how poor oral health can trigger acne and skin breakouts through bacteria, inflammation, and immune stress — and how smart brushing can protect both your smile and your skin.
